Written by Michael L. Bahrami-Hessari
Patient and Public Involvement Officer,
NIHR Southampton CRF
February 2020
In the months of November-December each year, NHS Trusts in Wessex try to gain insight on participants’ experience, motivations and feedback in joining clinical research through the national Patient Research Experience Survey (PRES). Each Trust in the region is given a target response. University Hospital Southampton (UHS) is the biggest PRES recruiter in the Wessex region and so was given a target of 301.
This felt a difficult task given that we only got around 105 responses in 2018.
So what happened? How did we improve our response rate?
I’d like to share with four things we did a little differently that may have contributed to our success which you may be able to apply to your own organisation.
1. Asking only essential, actionable questions
While it is tempting to inundate respondents with lots of questions just to cover all bases, longer questionnaires can be off-putting to people. For example, PRES 2018 had 17 questions but the CRN Wessex in coordination with members of the public decided to cut them down to 5 in 2019 which may have contributed to a three-fold increase in our responses at UHS. If you are struggling to decide if you want to include a question in a survey, ask yourself:

Will knowing this information result in something actionable?
2. Expanding our audience
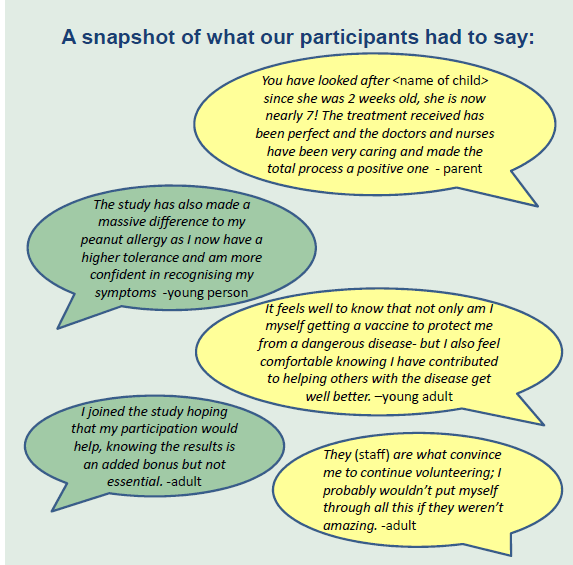
In past years, PRES only looked at responses of adults. This year CRN Wessex produced surveys for children (5-12yr); young persons (12-16yr) and carers. This allowed us to capture feedback from various audiences which resulted in a richer, stratified data set which revealed demographic-specific concerns that we otherwise couldn’t detect. For example, a common point of improvement identified by adults surveyed at the CRF was the lack of parking and pharmacy wait times while college students on a trial outside the CRF wanted to know more about the results of the study once it ended.
Research participants are a diverse group. Setting up mechanisms that recognise this diversity can result in a more robust dataset.
3. Gaining buy-in from all staff

While it is in the PPI Team’s remit to coordinate PRES at UHS, we recognise that we do not have clinical roles and do not see participants on a daily basis. Also, while our offices are based in the CRF, we realise that research teams are scattered throughout the Trust. This is why weeks before we started collecting survey responses, we talked to various nursing teams and explained to them
why and how we were conducting PRES and asked suggestions how they could assist us without impeding in their workflow. We put up posters with poly pockets to serve as collection points for completed surveys but also as reminders to staff that the survey period was ongoing. Finally, we had dedicated points of contacts from the various nursing teams who we periodically checked in with so that they could communicate to us their successes and challenges in collecting responses. To keep members of staff motivated, we sent an email updating them of our current numbers halfway through the collection period and another “celebratory” email once targets were reached.
Getting members of staff on board with a survey is the first step but keeping their momentum going, especially when you have yet to reach your goal, is just as important.
4. Giving respondents choices
In previous years we focused exclusively on collecting paper survey responses. However, not everyone is comfortable answering written surveys when they visit the Trust. For this last survey, we gave research participants the choice to either post back paper forms or answer the survey online through a link given by a research nurse. Recognising that lots of young people always have their mobile phones on them, we sent out SMS survey reminders after outreach visits to schools. As a result of this, online responses comprised 34% of our total responses- a significant increase from our 2018 numbers.
Research participants are busy. Giving them convenient alternatives helps with response rates.
Thank you to Michael and the team at NIHR Southamton CRF (pictured below) for sharing your tips on improving patient survey response rates.